My recent visit to the Czech Republic, sponsored by the Klicek Foundation, included a return to the Mendelova Nursing School in Novy Jicin. This time, Maria Fernanda Busqueta Mendoza joined us from Mexico, and 50 students participated in our seminar, making it a great opportunity for global learning and a multicultural exchange of ideas. As you can see from the first photograph, the students were a lively bunch, and they eagerly participated in the highly interactive time we spent together. Jiri Kralovec served as our interpreter and his son, Jiri, touted by Foto Video Magazine as this year’s hottest photographer on Instagram, documented our learning. Most of the photos below are his work.
Jiri and his wife, Marketa, started us off by sharing information about the importance of play for hospitalized children and the history of their efforts to bring hospital play to the Czech Republic. It has been a slow, uphill battle to change the hierarchal and disempowering bureaucracy of their medical system. I followed with an introduction to the field of Child Life, the role of child life specialists in hospitals, and the possibilities for collaboration with nurses. I spoke about the role of play and community in the healing process, before moving on to some illustrative activities.
Sharing our own memories of play is one way to deepen our appreciation for the role of play in our lives and in the lives of children. I asked the class to think about their own childhood memories, using their five senses — what do they remember about their play environment? Did play occur inside or outdoors, or both? Were they playing alone, or with others? Did they play with toys, loose parts, or their imaginations? Are there sounds, smells, tastes or textures associated with their memories? What feelings are evoked in sharing them? The students paired up and took turns both sharing and listening to one another.
 (photo by Jiri Kralovec)
(photo by Jiri Kralovec)

Armed wth a deeper awareness of the value of play, the students were now ready to learn a bit about how to make procedures less frightening for children. I have always wanted to use role play as a way to demonstrate all the things that can go wrong during a procedure, and how minor changes can make things easier for medical staff, children, and caregivers. I took this opportunity and asked for volunteers. One young man played the patient. We instructed him to lie down and asked three others to pin him down to the table, much like medical personnel are likely to do when a child receives an IV. We demonstrated how the very act of being forced into a prone position increases one’s sense of vulnerability and loss of control.
 (photo by Jiri Kralovec)
(photo by Jiri Kralovec)
Add to that several adults talking at once, loudly over any protests you might make, telling you to stay still, not to cry, to be a big boy, not to look…. and you get the picture. Chaos, stress and shame accumulate to make for a disastrous experience for all.
 (photo by Jiri Kralovec)
(photo by Jiri Kralovec)
But there are some simple things that nurses can do, either alone or in partnership with play specialists, to change the outcomes of such procedures. It doesn’t mean that the child won’t cry, but it is more likely that the child won’t suffer emotional trauma, will return to baseline quicker, and the nurses can feel more successful and less like they are causing the child undue suffering.
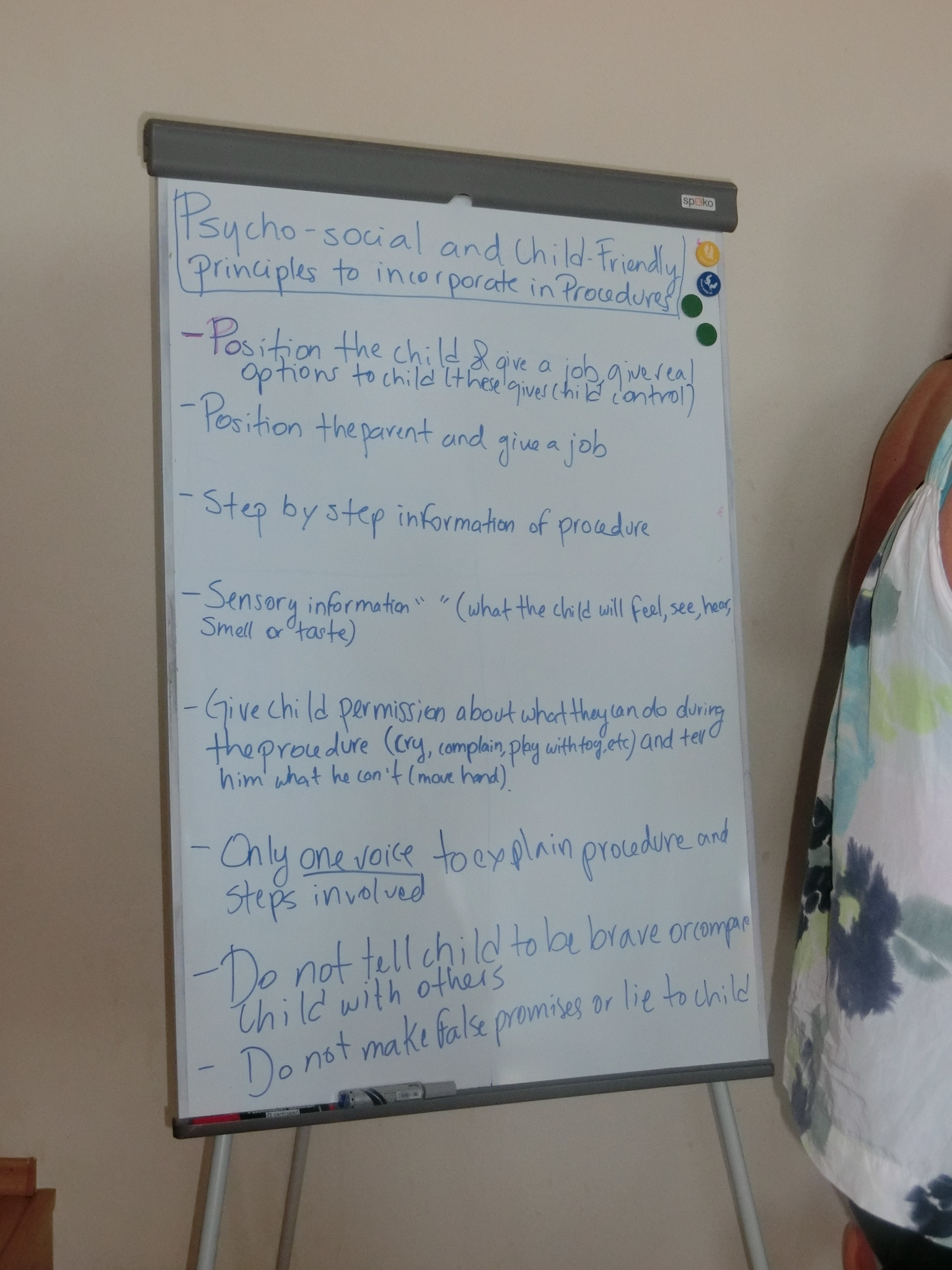
With these tips in mind, the students enacted a better case scenario, where the parent has a supportive role in positioning the child for comfort. The child is upright and held in a calming hug, rather than being restrained on the table. The child is given some choices, such as which hand to try first for the IV (the non dominant hand is preferable), and whether to watch the procedure or use a toy or book for distraction.
- Electing one person to be the voice in the room,
- encouraging the child to breathe deeply and slowly,
- narrating each step of what the child will feel,
- explaining how a tiny plastic catheter, not the IV needle, remains in the child’s hand to deliver medicine,
- staying away from comparative or shaming statements,
- and showing empathy
are all ways to provide psychosocial support, making the experience less traumatizing and painful for the child. Accumulated painful and traumatic medical experiences can make children phobic and avoidant of medical care.
 (photo by Jiri Kralovec)
(photo by Jiri Kralovec)
 (photo by Jiri Kralovec)
(photo by Jiri Kralovec)
We also spoke about non-pharmacological pain prevention and reduction. The interactive component of our lecture surely made our important information memorable. The action and laughter surely made more of an impression than a power point! We all reflected together about how even adult patients can benefit from choices, information and empathy.
Back to the topic of play, we explored ways for the nurses to instill playful interactions into their communication with pediatric patients. Rapport building and distraction through the use of hand games is one way that they can put a child at ease. I demonstrated several hand games, and asked them to show me some of theirs as well.
 (photo by Jiri Kralovec)
(photo by Jiri Kralovec)
Our time with these wonderful students ended all too soon. We posed outside of the school for a photo with some of the Klicek Foundation hospital play specialists before heading to the historic square down the street. Around every corner of this country is a beautiful scene, no matter where you are!
 (photo by Jiri Kralovec)
(photo by Jiri Kralovec)
 (photo by Jiri Kralovec)
(photo by Jiri Kralovec)


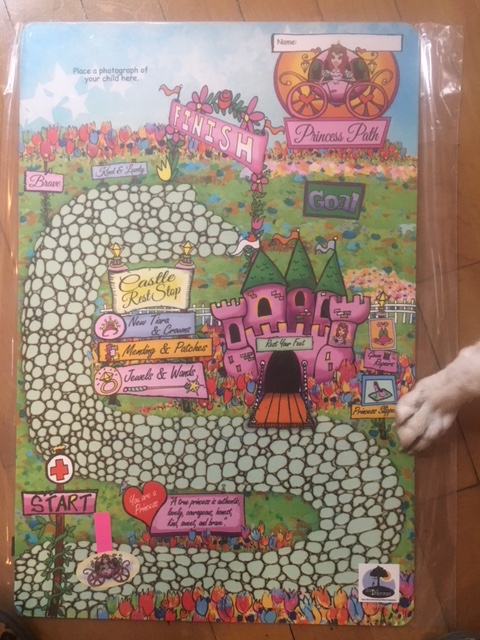

 Guest Blogger Heather Beal is a military veteran with 23 years of crisis management and operational planning experience that she draws upon daily in her battle to raise two well-prepared, happy, curious, and intelligent children. As a trained emergency manager and parent, she saw the need to provide age-appropriate disaster preparedness information to young children in a way that empowered rather than frightened them. She is currently writing additional books to cover a greater spectrum of potential disasters children may face.
Guest Blogger Heather Beal is a military veteran with 23 years of crisis management and operational planning experience that she draws upon daily in her battle to raise two well-prepared, happy, curious, and intelligent children. As a trained emergency manager and parent, she saw the need to provide age-appropriate disaster preparedness information to young children in a way that empowered rather than frightened them. She is currently writing additional books to cover a greater spectrum of potential disasters children may face.


 (photo by Jiri Kralovec)
(photo by Jiri Kralovec)
 (photo by Jiri Kralovec)
(photo by Jiri Kralovec) (photo by Jiri Kralovec)
(photo by Jiri Kralovec)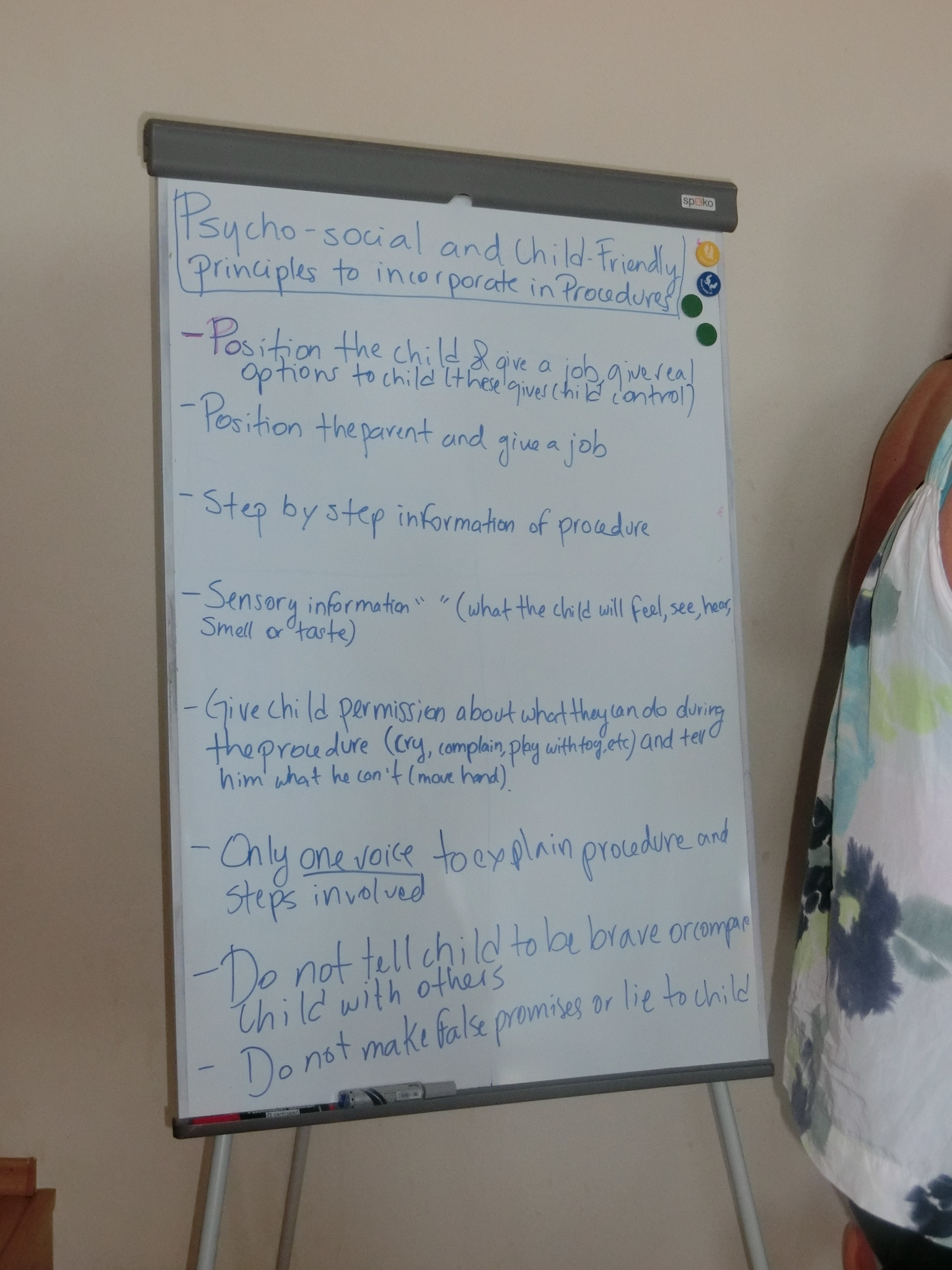
 (photo by Jiri Kralovec)
(photo by Jiri Kralovec) (photo by Jiri Kralovec)
(photo by Jiri Kralovec) (photo by Jiri Kralovec)
(photo by Jiri Kralovec) (photo by Jiri Kralovec)
(photo by Jiri Kralovec) (photo by Jiri Kralovec)
(photo by Jiri Kralovec)