I have not blogged in almost two years. The everyday stress of the Pandemic coupled with work and personal obligations have siphoned much of my creative energy. But I feel called upon today to use my voice and my blogging platform to address something that we all need to talk about. I have heard through the social media grapevine that some child life specialists are asking for CCLS silence on social media regarding “political posts”, specifically in response to the overturning of Roe vs. Wade by the Supreme Court last week. I am here to say that as healthcare advocates, we owe it to our profession and to our patients and families to engage in these hardest of conversations. If we don’t, we will stay in our own opposite corners and lessen the possibility of joint intersubjectivity, learning, understanding, and ability to meet the needs of the children and families in our care.
In order to do this peaceably and professionally, we can keep these guidelines in mind:
- Speak from an “I” place of sharing your beliefs and opinions.
- Avoid “You” statements.
- Seek to understand more than to be understood.
- Avoid any and all vitriol (Telling people to shut up, step down, calling people names).
- Speak with a gentle understanding that there are many viewpoints and beliefs and values that differ from yours.
- No opinions are ever changed by shouting someone down and insulting them.
- Start from the assumption that everyone in the room cares about the health of children and families.
- Be accountable for your words – posting anonymously makes it more likely that you will not edit yourself and use your anonymity to shout someone down.
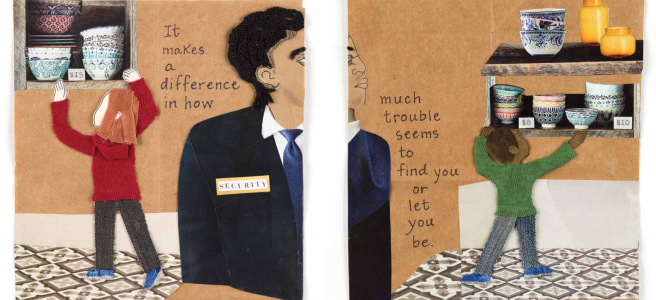
- Be aware of your level of privilege, and the impact it may have on your audience.
- Use your social media platform to make a safe space for conversation – @ChildLifeTherapy does this in a wonderful way on Instagram.
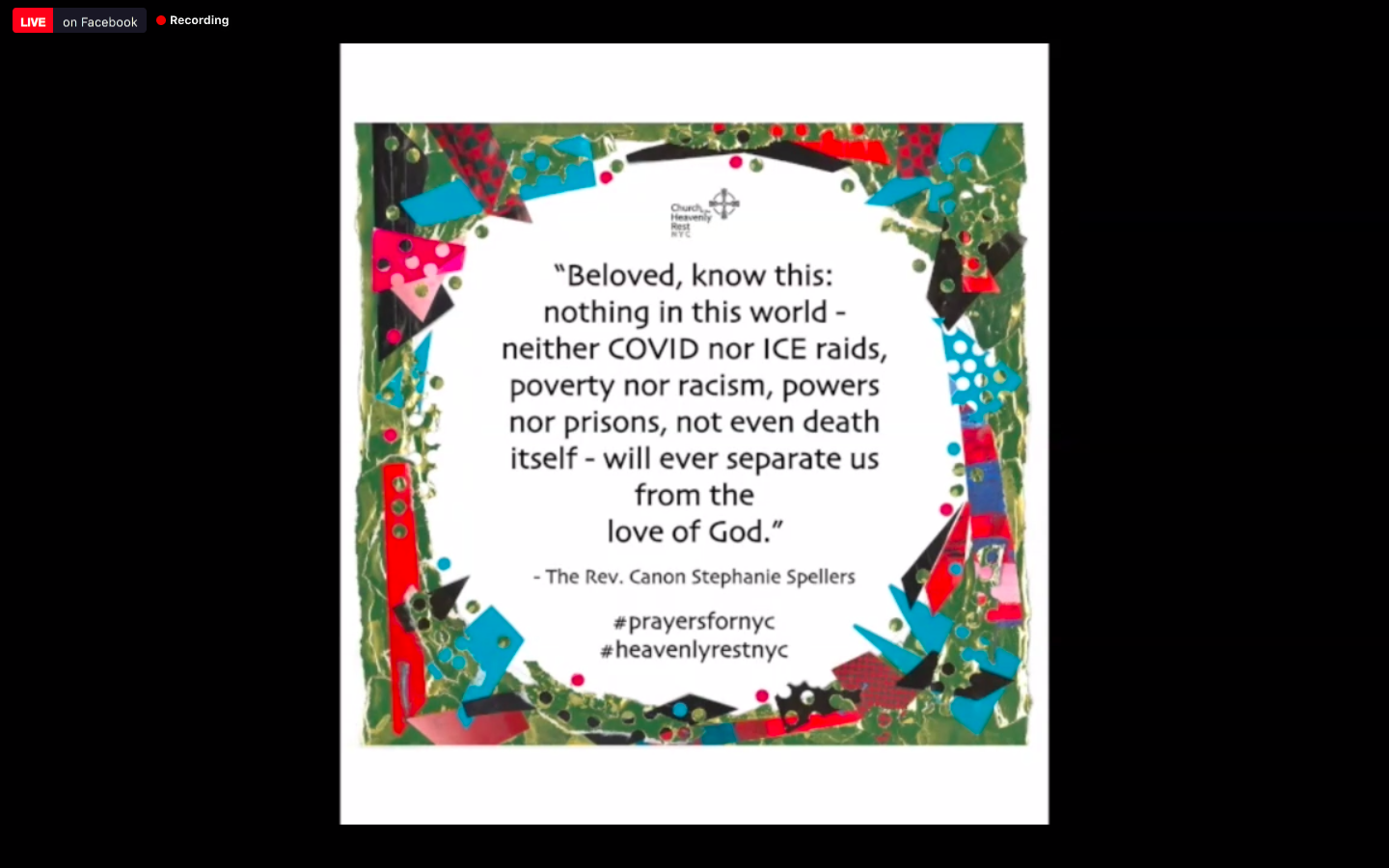
- Understand that religious values that guide opinions are deep and sacred things that vary hugely in how they define the beginning of life.
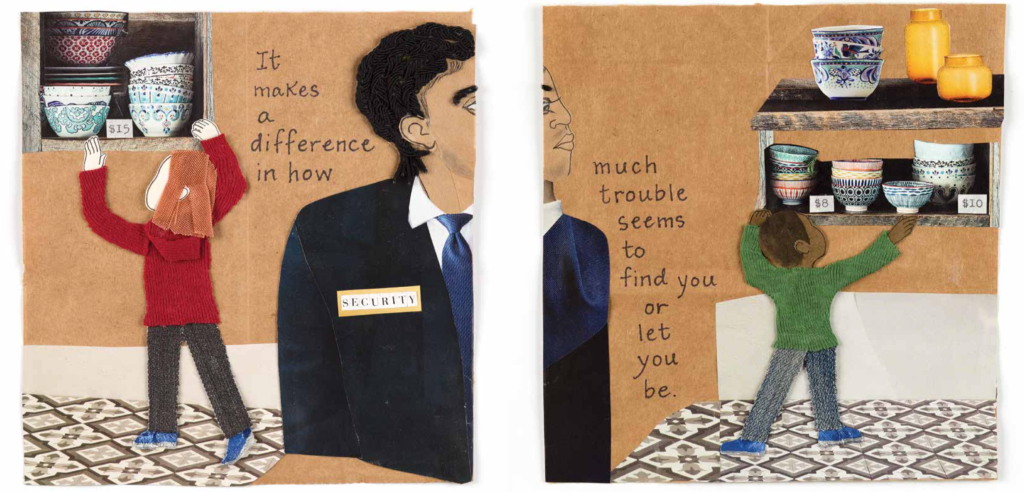
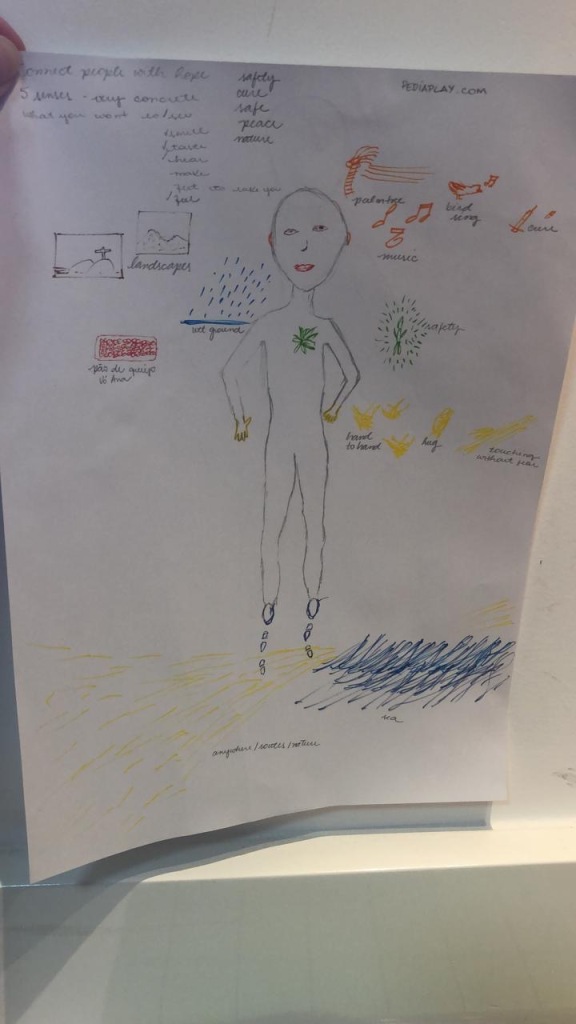
- Do regular check-ins with yourself to see if you are following your own True North, and helping others do the same.
Fact: The JUNE 24, 2022 DOBBS V. JACKSON WOMEN’S HEALTH ORGANIZATION decision will negatively affect access to life-saving healthcare for many women and girls, with the intersection of race, age, and poverty putting our less privileged and oppressed populations at the highest risk for mortality.
Questions to consider:
- What does this mean for child life specialists who care for children and families in hospitals each and every day?
- What does this mean for child life specialists who celebrate the overturning?
- What does it mean for those specialists who rage against it?
- How can we find common ground to ensure that we are fulfilling our ethical responsibilities to our patients (and colleagues)?
- What do our competencies tell us about our ethical duties to all patients?
- What extra training and support might we need to fulfill our duties in serving patients and families impacted by the change in healthcare access?
- How do we manage our personal fears about our own bodies and access to healthcare?
- How do we serve patients and families who have different religious, political, and personal beliefs and values than we do?
- What is your True North and how do you balance it with serving patients and families?
- Add your own many questions here……………
These questions can keep us on the right path. This path is new and daunting to most of us, but these conversations are the same ones we have always had as a profession about race, LGBTQ+ issues, immigration issues, and culturally-informed, trauma-informed care. We may need to stretch ourselves, but we have the built-in elastic with which to do this! More bifurcation and strife will not make us better providers.
In the words of Mother Theresa:
Lead me from Death to Life, from Falsehood to Truth.
Lead me from Despair to Hope, from Fear to Trust.
Lead me from Hate to Love, from War to Peace.
Let Peace fill our Heart, our World, our Universe.
Peace Peace Peace